Background: The Blood Cancer UK TAP CLARITY trial for relapsed or refractory CLL combined IBR with VEN in order to eradicate detectable disease with a plan to stop therapy early if measurable residual disease (MRD) <0.01% (MRD4) was achieved in the peripheral blood (PB) and bone marrow (BM).
Aims: To provide long term follow up data for the combination of IBR and VEN for R/R CLL patients. IWCLL response status and MRD responses status at the 38 month time point are now presented in this abstract.
Methods: CLARITY is a Phase II trial combining IBR with VEN in 50 patients with R/R CLL. After 2 months of IBR, VEN was added initially at a daily dose of 10mg or 20mg/day escalating weekly to a final daily dose of 400mg/day. CLL MRD was quantified using >6 colour ERIC-standard flow cytometry (detection limit 10-5/0.001%). Paired PB & BM samples were assessed at months 8, 14, 26 and longitudinal PB samples were taken at multiple time points. Fifty-four patients were recruited from May 2016 to November 2017. The median number of prior therapies was 1 (range: 1-6). 20% patients had del(17p); 25% del(11q); 75% had unmutated IGVH. Four patients that discontinued treatment due to ibrutinib-related adverse events in the first 8 weeks before starting VEN were replaced so that, in total, 50 patients received the combination of IBR and VEN. The interruption of therapy was indicated following confirmation of a CR according to the iwCLL2008 criteria and MRD reduction <10-4 CLL cells in PB and BM (MRD4). MRD4 at month 8 indicated to stop IBR and VEN at month 14, MRD4 in PB and BM at month 14 and/or at month 26 indicated to stop IBR and VEN at month 26, while MRD detectable at month 26 indicated to stop VEN only and to continue IBR until progression or toxicity. The trial protocol was amended later in Jan 2019 to allow patients, who had not obtained an MRD4 at month 26, to have an extra 12 months of VEN in addition to IBR.
Results:
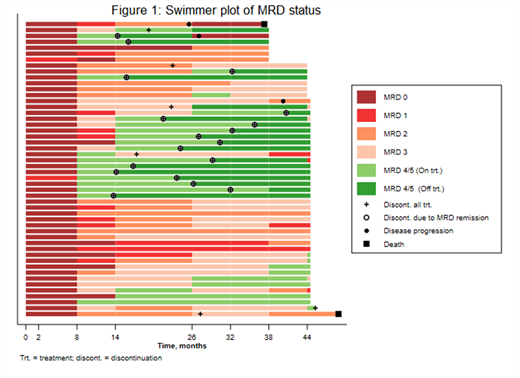
Of the 50 evaluable patients recruited to the study, 23 patients stopped both treatments at or before M38; the majority due to achieving MRD4 (17/23). 27/50 patients were still receiving at least one trial treatment at this time point, with M38 response data pending for 11 patients. Of the 27 evaluable patients on treatment, the overall response rate (ORR), comprising of 10 patients with CR and 3 with CRi, was 81% compared to an ORR of 91% in the 36 patients receiving at least one trial treatment at M26 respectively. One additional patient discontinued treatment due to MRD negativity after M38. Of the 18 patients stopping due to MRD negativity, 14/18 continue to have <0.01% MRD.
Overall, MRD responses continued to improve after the first year of combination treatment with 24/50 (48%) patients achieving MRD4 in the BM at month 26 compared to 20/50 (40%) at month 14. After 4 months of combination, the median log CLL depletion was 2.9 (range 0.2-4.8) for patients achieving <0.01% MRD at month 26 vs. 1.4 (range 0.1-4.6) for patients with ≥0.01% MRD at month 26. Disease depletion from month 4 to month 8 was slower in all groups, with a median log CLL depletion of 1.1 (range 0.1-2.9) for patients achieving <0.01% MRD vs 0.7 (-0.4-2.3) for those with ≥0.01% MRD at month 26 respectively. After month 8 (6 months of combined IBR+VEN), patients with ≥0.01% MRD typically showed <0.5log depletion/year subsequently. Of 20 evaluable patients with <0.01% MRD at month 38, MRD depletion had already been achieved at 6 months of combination IBR+VEN in 7/20 (35%), at 12 months in 14/20 (70%), and at 24 months in 18/20 (90%).
There was only one case of biochemical TLS. Other side-effects were mild and/or manageable, most commonly neutropenia (3/37 grade 2, 34/37 grade 3/4). Two Suspected Unexpected Serious Adverse Reactions (SUSARs) were reported (abdominal pain and pemphigus), 44 Serious Adverse Events (SAEs), and 1153 Adverse Events (AEs) (of which 141 were grade 3 or 4) were reported.
Summary/Conclusion: After 38 months, the response to IBR+VEN is sustained despite planned discontinuation of therapy in MRD negative patients. The initial rate of disease depletion (during the first two months of combined IBR+VEN exposure) is highly predictive of longer-term response to combination IBR+VEN treatment in relapsed/refractory CLL. Patients who do not show rapid disease clearance and have persistent MRD after 12 months of combination IBR+VEN usually have stable or slowly decreasing disease levels akin to that seen in IBR monotherapy. These data will be updated at ASH 2020.
Hillmen:AbbVie: Speakers Bureau; Janssen: Speakers Bureau; Gilead: Speakers Bureau; Pharmacyclics: Other: Financial or Material spport; Morphosys: Other: Consulting fees; Sunesis: Other: Consulting fees. Brock:Invex: Other: Consulting and speaker fees; Merck: Other: Reimbursement of costs; Eli Lilly: Other: Consulting and speaker fees; AstraZeneca: Current equity holder in publicly-traded company; GlaxoSmithKline: Current equity holder in publicly-traded company. Schuh:Illumina: Other: Consulting fees; Abbvie: Other: Consulting fees; Gilead: Other: Consulting fees; Roche: Other: Consulting fees. Pettitt:Roche: Honoraria, Other: Hospitality, Research Funding; Napp: Research Funding; Celgene: Other: Hospitality, Research Funding; Chugai: Research Funding; Gilead: Honoraria, Other: Hospitality, Research Funding; Kite: Honoraria, Other: Hospitality, Research Funding; GSK: Research Funding; Novartis: Research Funding. Gribben:Janssen: Honoraria, Research Funding; AstraZeneca: Honoraria, Research Funding; Abbvie: Honoraria; Celgene: Research Funding. Patten:Roche: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Honoraria; Gilead: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Astra Zeneca: Honoraria; AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Bloor:Abbvie: Consultancy, Honoraria, Other: Conference Funding, Speakers Bureau; Janssen: Consultancy, Honoraria, Other: Conference Funding , Speakers Bureau. Fox:Celgene: Current equity holder in publicly-traded company; Sunesis: Current equity holder in publicly-traded company; Atarabio: Current equity holder in publicly-traded company; Abbvie: Current equity holder in private company, Current equity holder in publicly-traded company; Gilead: Current equity holder in private company, Current equity holder in publicly-traded company; Adienne: Current equity holder in private company, Current equity holder in publicly-traded company; Roche: Current equity holder in private company, Current equity holder in publicly-traded company; AstraZeneca: Current equity holder in publicly-traded company; Takeda: Current equity holder in private company, Current equity holder in publicly-traded company. Forconi:Roche: Honoraria; Janssen: Honoraria, Other: Fees for cosulting or advisory role, received travel and expenses, Speakers Bureau; AbbVie: Honoraria, Other: Fees for cosulting or advisory role, received travel and expenses, Speakers Bureau; Gilead: Research Funding; Astra Zeneca: Other: Fees for cosulting or advisory role; Menarini: Other: Fees for cosulting or advisory role; Novartis: Honoraria. Rawstron:BD Biosciences (Intrasure): Patents & Royalties. Hillmen:Alexion: Consultancy, Research Funding, Speakers Bureau; AstraZeneca: Consultancy, Speakers Bureau; Acerta: Other: Financial or material support; Roche: Consultancy, Other: Financial or material support, Research Funding, Speakers Bureau; AbbVie: Consultancy, Other: Financial or material support, Research Funding, Speakers Bureau; Pharmacyclics: Other: Financial or material support, Research Funding; Janssen: Consultancy, Other: Financial or material support, Research Funding, Speakers Bureau; Apellis: Consultancy, Research Funding, Speakers Bureau; Gilead: Other: Financial or material support, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal